Nine significant moments in the history of the hospital built for £226million for the Maidstone and Tunbridge Wells (NHS) Trust
- A Care Quality Commission report early in 2015 ‘found leadership within the trust was not robust’. It also said each of its two hospitals, Tunbridge Wells and Maidstone, ‘requires improvement’.
- The trust was heavily criticised in 2007 by the Healthcare Commission for the way it handled a major outbreak of the bacterium C. diff. It’s estimated that about 90 patients ‘definitely or probably’ died as a result of the infection. The outbreak was subsequently connected to the financial reorganisation that the trust was undergoing, including the private finance initiative (PFI) that built the showcase hospital.
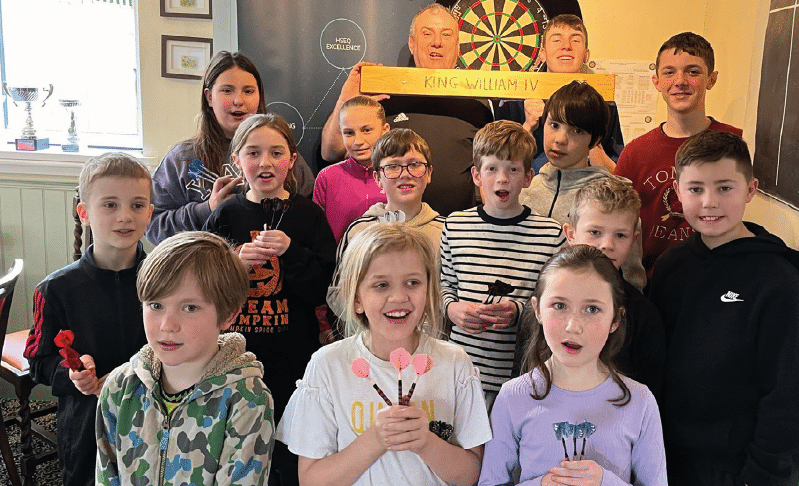
- A new 38-bed ward at Pembury opened in March to ease pressure on stretched emergency facilities. The £3.3million Acute Medical Unit (AMU) has two single rooms and nine four-bed bays, designed to treat patients for up to 48 hours before discharge or transfer. The unit’s team includes three consultants and 56 nurses.
- In the opening two months of this year an ‘unprecedented’ demand for services led to the cancellation of 350 elective surgery operations. Some patients were transferred to the private sector.
- A Times Freedom of Information request last year showed that in three years the trust spent almost £70million on agency and temporary staff. Agency staff are more expensive than regular staff. Local MP Greg Clark called the figure ‘worrying’.
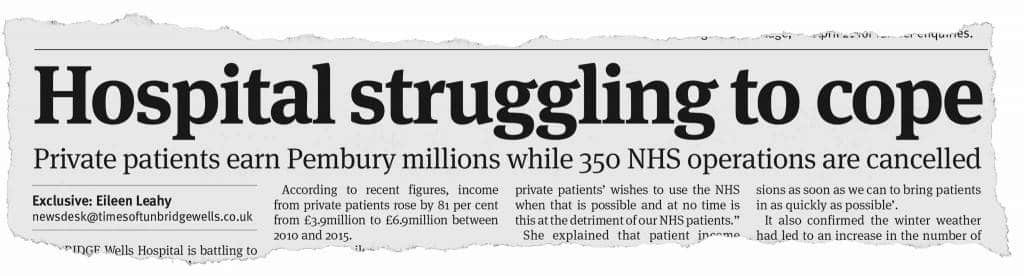
The Times of Tunbridge Wells reported on difficulties on March 2
- Figures released in June show that, overall, patients rate the Tunbridge and Maidstone hospitals ‘highly’ when it comes to staff and care. A record number of adults (709) shared their views about care they received as part of a national survey. They were all discharged from hospital in July 2015.
- During 2014 the trust paid interim finance director Ian Miller £250,000 for five months’ work. The money went to his consultancy business The Maxentius Partnership. The trust said the expense was justified in order to ‘achieve £23.5million in efficiency savings without impacting patient care’.
- Last year the trust became the first in the NHS to be charged with corporate manslaughter when teacher Frances Cappuccini (30) died after giving birth by emergency Caesarean section. The judge ruled there was no evidence of gross negligence and the case collapsed.
- The Health Service Journal named the trust as one of the top 100 to work for in 2015. At the time it had 5,000 full-time equivalent staff and a sickness absence rate of just under four per cent. The majority of staff (73 per cent) recommended it as a place for treatment.